Prior to adopting a low-carbohydrate diet for controlling type-1 diabetes my wife had a high lipid panel. Her doctor wanted her to take a statin drug. Nicole refused. As the Mayo Clinic states “statin use could cause an increase in the level of enzymes that signal liver inflammation.” They also say that one of the “most common complaints of people taking statins is muscle pain.” Such muscle pain can lead to rhabdomyolysis can cause “liver damage, kidney failure and death.” Oh, and statins can also cause a “mild increase in sugar value.”
Despite these dire side-effects, I remember that while Nicole was hospitalized (about 12 years ago) a nurse berated her for not taking Lipitor. (Lipitor is such an interesting name. Sounds like a villain from a comic book. Wasn’t Lipitor Spiderman’s arch-enemy?)
When Nicole switched to a high-fat, moderate protein, low-carb diet her lipid panel improved. Her HDL (the “good” cholesterol) remained high; her triglycerides came down into normal range; but her LDL (the “bad” cholesterol) was off the chart.
Many of the low-carb gurus argue it’s only dense LDL that’s the problem. Most lab tests don’t differentiate. According to a 1988 study in the Journal of the American Medical Association “small, dense LDL particles [were] significantly associated with a threefold increased risk of myocardial infarction.” Myocardial infarction is doctor-lingo for a heart attack. Does this mean only light and fluffly LDL is harmless? Or does it just mean that light and fluffly LDL is simply less harmful?
Regardless, due to other problems Nicole was facing with the low-carb diet she started introducing some grains. As she added starches, however, her triglycerides also rose into the danger zone and the LDL became even higher. (She was still eating plenty of fat and protein. )
So that didn’t seem to working out so well.
In December, however, Nicole began testing a completely different approach: High-carb, low protein, low-fat. The carbs have been coming from whole-grains (rice, oats, buckwheat), legumes (sprouted lentils, chick peas and pinto beans), high-carb vegetables (yams, parsnips, carrots…) and a little bit of fruit (apples, raisins…). The fat is kept to a minimal – about 60g (2oz.) of nuts and seeds a day. Other than fat naturally present in food, there are no added oils, butter, whipping cream, lard, etc.
She’s also not eating any animal products at all. Hence the protein levels are quite low – whatever she gets from the nuts, seeds and beans.
Now, I’ve heard many different stories about how people responded to vegan diets. Some claim they have perfect lipid panels while others had the worst lipid panels of their life. Of course, there are many different versions of a vegan diet. It may not come as too much of a surprise if the lipids are high on a diet consisting of soy ice cream, jars of peanut butter, whisky and vegan brownies. But what about a diet, like Nicole is following right now, consisting of unprocessed, natural foods?
Well, Nicole had a blood test done recently and the results were certainly noteworthy. albeit anecdotal. The entire lipid panel was in normal range. HDL stayed up, while LDL and triglycerdies came down, as you can see here….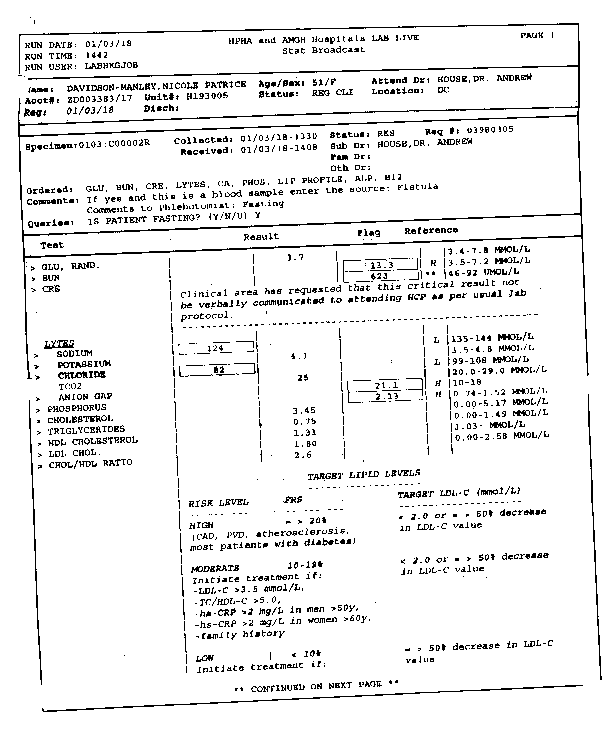
Many might argue that cholesterol is so darn good for you that you just can’t have too much. Whether this is true or not is always going to be open for debate. Nonetheless, in Nicole’s case at least, it is very interesting to see that someone with T1D for 40+ years, who is on dialysis, could so easily bring her lipids within (what is widely considered) normal range by dietary changes alone. Likewise, her blood pressure is also within completely normal range, as I wrote about here.
Not only was her lipid panel looking like that a of a teenager, but mine has also normalized. My last test in 2016 showed the LDL had crept up into the “danger” zone. Having now followed the same vegan diet (as Nicole is following) for the last five months, a blood test I had done last week showed likewise normal cholesterol levels.
Even more shocking was that my HgbA1C went from the 5.5% to 4.8%. Yes, 4.8% eating a diet where more than 80% of the calories is coming from carbohydrates. (When it was 5.5% I was eating a low-carb diet.)
Nicole’s blood sugars have likewise not become any less controllable. She has’t had an A1C done recently to confirm, however.
So far the lipo-toxicity theory I wrote about previously seems to be holding true. It does indeed appear that human livers (like those of herbivores) may produce all the cholesterol needed to function. Any dietary intake of animal fat may simply be clogging glucose receptors, giving the liver excess cholesterol to clear out and impeding the transport of blood throughout the cardiovascular system.
With all the challenges Nicole faces with type-1 diabets and kidney failure it does feel like a relief and victory to see her lipid panel, blood sugars and blood pressure in such a safe place. If removing animal products, oil, salt and sugar is all that is needed to minimize the risk of a heart attack and stroke, it may give people with T1D the edge they need to live a long and healthy life.
And if we consider how small the blood vessels to the beta cells are I’d also wager that clearing the blood of congesting cholesterol may be critical to their recovery.
Thinking outside the T1D Matrix,
–John C. A. Manley
P.S. For one perspective on how to manage T1D with a plant-based diet you can read Dr. Neal Barnard’s book on diabetes. It’s written for people with T2D, but by combining Dr. Barnard’s diet with Dr. Bernstein’s insulin regimen, it seems like people with T1D can obtain a HgbA1C of 5.5% or lower. Dr. Barnard’s book is available from amazon.com, amazon.ca, and amazon.co.uk).
P.P.S. We’re almost at the $9k mark for our fundraiser. Special thanks to all the loyal readers who’ve contributed (some on multiple occasions). There’s still a lot to be raised ($40k). Please consider even a small donation at kidneykarma.com.
